 Blogs
Blogs
Clinical research carries significant risks and numerous obstacles that must be overcome to achieve success. Identifying the ideal Contract…
 Blogs
Blogs
Neurodegenerative diseases affect millions worldwide. Fifty million people are living with Alzheimer’s disease or other dementias. Although Alzheimer’s disease is one of the most recognized, it is just one of many neurological disorders, such as Multiple Sclerosis, Parkinson’s, or Huntington’s disease. These conditions lead to a…
 Blogs
Blogs
ICH M10 (International Committee of Harmonization Multidisciplinary guideline) provides guidance on bioanalytical method validation and study sample analysis for the measurement of chemical and biological human drugs and their metabolites in biological samples. Such pharmacokinetic/toxicokinetic data serve as the basis for regulatory decisions on the safety, dosage, and…
 Blogs
Blogs
Being that it is a relatively “niche” segment of the industry, there are several key areas that need to be considered in the field of molecular services related to cell and gene therapies. First and foremost, it is important to recognize that regulatory guidelines within this field are…
 Blogs
Blogs
Anyone who has been following KCAS for any amount of time has likely heard us discuss the advantages of Hybrid LC-MS/MS for the bioanalysis of large molecules. As pioneers in the technology for many years, KCAS has become a strong proponent of working with our customers to demonstrate the quality…
 Blogs
Blogs
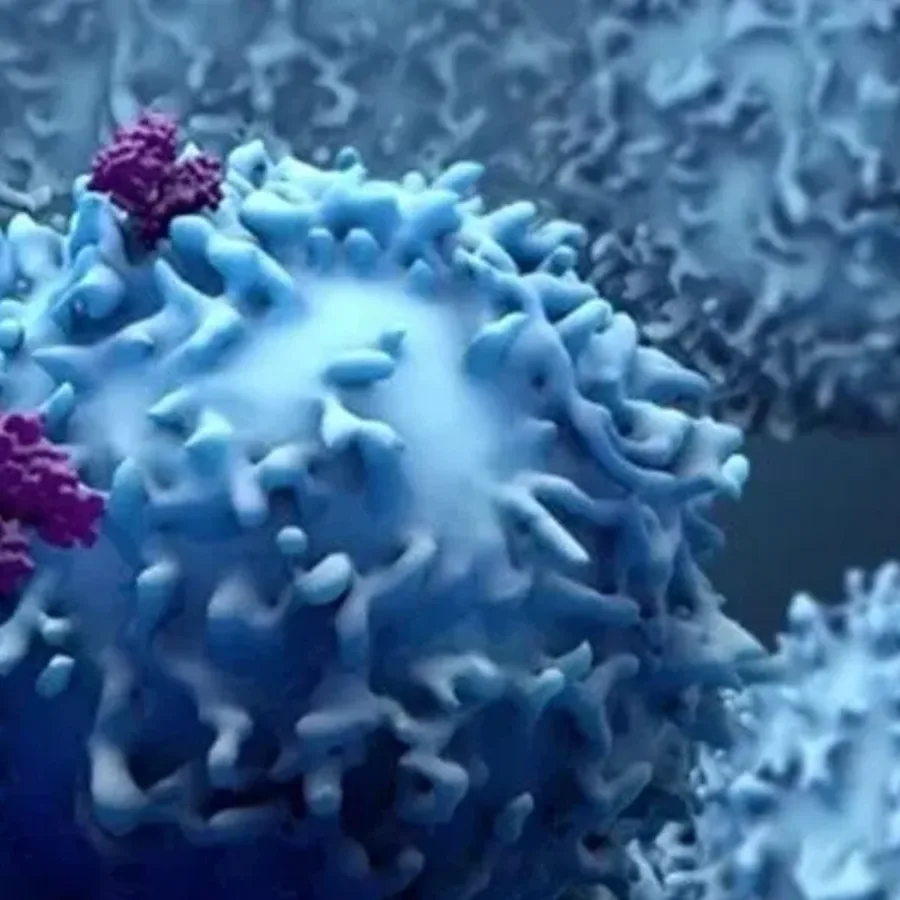
Understanding the interactions between drugs and biological systems is critical for the success of a new drug. One key tool in this process is functional assays. Functional assays are customized assays that evaluate the impact of drugs on the functionality of cells. They test for a drug’s specific biological mechanism…
 Blogs
Blogs
In 2022 we had 42 FDA Drug Approvals and 3 were Gene Therapies using a viral vector. 2 of the approvals in 2022 were AAV based. The third is manufactured by adding functional copies of the transgene to the patient’s own Hematopoietic Stem Cells (HSCs)…
 Blogs
Blogs
With 2022 firmly planted in our rearview mirror, and the planning for the new year essentially complete, we all look forward to a new year with cautious optimism as we wait to…
 Blogs
Blogs
Cell and Gene Therapies (CGTs) has an estimated market size value in 2022 of USD 8.22 billion and a revenue forecast in 2030 of USD 24.5 billion. This is a CAGR (compound annual growth rate) of 14.6% from 2022 to 2030. Needless to say, the…
 Blogs
Blogs
Dose Formulation Analysis is an essential step in regulated nonclinical studies. Robust analytical methods, rapid turnaround, and efficient communication helps deliver your GLP studies’ dose formulation analysis results on time…
 Blogs
Blogs
Due to its ability to analyze multiple parameters across different cell types within a sample, flow cytometry provides rich and clinically valuable data sets from even small volumes of blood. However, flow cytometry is a challenging platform to master, and requires significant investment in equipment and technical training.
 Blogs
Blogs
KCAS established our Clinical Sample Kitting team in the early 1990s in response to shortcomings we observed in the collection techniques in trials where we were providing bioanalytical support. As the group has evolved, our aim has been to provide the flexible, custom service that…