 Blogs
Blogs
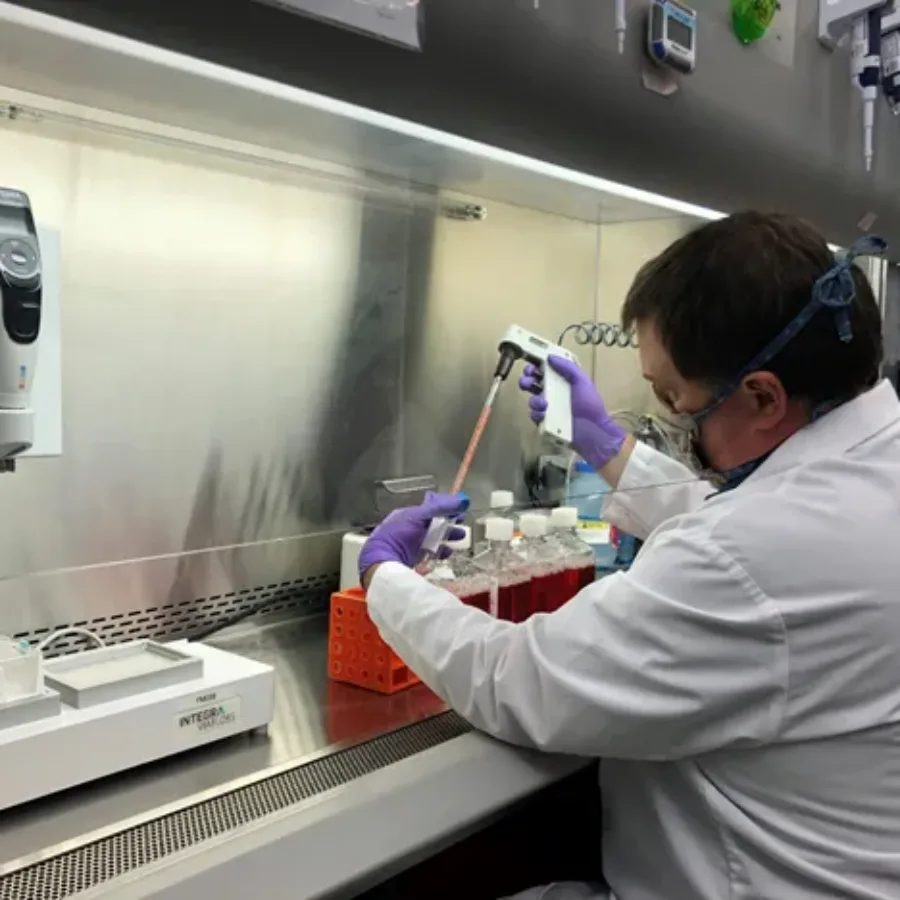
Assay validation is required during the development of new drugs or biologics in order to be in compliance with regulatory requirements for all studies that are not considered research/exploratory in nature. Beyond compliance, what is the point of assay validation? Assays must be precise, robust, and specific during use in preclinical studies and clinical trials in order to assure that drug candidates can be accurately evaluated for safety and efficacy. Validation plans assure that an assay will work reliably, even if an assay is run at different sites or by different users. Consider these other elements of assay validation to understand why it is a critical to preclinical and clinical research: Fit-for-purpose strategy: Each validation plan determines if an assay is made to be fit-for-purpose for a given client’s evaluation needs. Assays can be customized to meet the specific needs of a preclinical screening or clinical trial and fit-for-purpose validation assures that reliable data can be obtained from assay. Test scripts: Test scripts are a series of procedures to be executed during a validation in order to determine if an assay satisfies the necessary specifications or to reveal errors that must be addressed. Running test scripts is essential to the development and continued reliability of a validated assay. GLP compliance: Assay validation must be carried out under the same conditions as will be used for routine assay use. Good laboratory practices (GLP) conditions are needed for many preclinical and clinical applications, and routine quality assurance/quality control monitoring may also be necessary. Be aware of these special circumstances during assay validation. Validation is so much more than a regulatory hurdle. Validation gives you confidence that an assay will yield reliable results that can be trusted to make critical decisions for advancing drug candidates or evaluating clinical efficacy.
 Blogs
Blogs
Flow cytometry has been developed and used as a clinical tool since the invention of the first cytometers in the 1970s. At present, flow cytometry is considered essential for many routine clinical diagnostics, including assays for leukemia and lymphoma, stem cell enumeration, solid organ transplantation, HIV infection status, immunodeficiencies, and hematologic abnormalities. Many scientists involved in clinical trials or drug development are faced with developing clinical flow cytometry assays for multiple phases of clinical development. If you find yourself starting to plan a clinical flow cytometry assay, here are the top 3 issues to think about as you plan your experiment.
 Blogs
Blogs
Many scientists performing preclinical and clinical research hit a point when they need to have an assay validated. You may have painstakingly developed and perfected a particular assay, but now you must put it through the rigors of validation for it to be considered a “validated assay.” The basic principles of assay validation were described in an earlier blog post, but how do you know you if you need an assay validated? Use these questions as a guide to help you figure out your validation situation and get a little less vexed about validation.
 Blogs
Blogs
Flow cytometry is an elegant and powerful tool that has been critical to understanding the immune system and advancing the development of immune-based therapies. Critical to many studies, and essential for FDA filings, is the development and documentation of a validated assay. While most flow cytometric assays fall into the “quasi-quantitative” category according to FDA guidelines, there are some assays that can be quantitative and even qualitative.
 Blogs
Blogs
The idiom, garbage in, garbage out applies to many areas of scientific research, including flow cytometry. Good sample preparation is critical to accurate and sensitive cytometry analysis of cells, wherever their origin.
 Blogs
Blogs
Flow cytometry assays are important for preclinical and clinical research, however, it is vital to understand the level of compliance required for the stage of research you are completing. Flow Cytometry assays completed for toxicology and safety assessments are required to be in compliance of Good Laboratory Practices (GLP), on the other hand, basic research or discovery/exploratory studies can be non-GLP. GLP refers to a set of standards for laboratory studies to be planned, performed, monitored, reported, and archived. Preclinical and clinical studies must be GLP-compliant in order to be submitted for review by regulatory agencies like the FDA. Consider these three points if you find yourself in need of a GLP-compliant flow cytometry assay.
 Blogs
Blogs
What is the primary role of Natural Killer (NK) cells? Natural killer (NK) cells are the predominant innate immune cells that mediate anti-tumor and anti-viral responses, and therefore possess good clinical utilization (Abel et al. 2018). Natural killer cells comprise 10–15% of peripheral blood lymphocytes and classically display a half-life of approximately 7–10 days in the circulation (Moretta et al. 2000).
 Blogs
Blogs
Tissue and Non-Liquid Matrices (such as cell lines, red blood cells, PBMCs, bone marrow aspirates, and suspension cells) are valuable matrices[] to test for biomarkers (PD) and drug levels (PK). Testing of tissues and…
 Blogs
Blogs
Pharmacodynamics (PD) is defined as the study of the biochemical and physiological effects of drugs and the mechanisms of their actions. Where pharmacokinetics looks at how the organism processes the drug, pharmacodynamics studies how…
 webinars
webinars
Join us Tuesday November 10, 2020 at 11am EST| 8am PST| 4pm CET| 5pm CET Bioanalytical liquid chromatography–mass spectrometry (LC–MS) for small molecules is often referred to as a routine technology. That perception may be true for many drugs, but as pharmaceutical companies move into new areas, more projects may…
 Blogs
Blogs
Dose Formulation Analysis is an essential step in regulated nonclinical studies to ensure correct doses are administered to underpin toxicokinetic assessments. Based on years of experience, KCAS has built a stand-alone team dedicated to…
